Command Palette
Search for a command to run...
Li Jianping, Vice President of Peking University Hospital: Using AI to Solve the Difficulties, Bottlenecks and Pain Points of Clinical Myocardial Ischemia Prediction

On June 14, 2024, the 6th Beijing Zhiyuan Conference opened at the Zhongguancun Exhibition Center. Experts and scholars from home and abroad held wonderful speeches and dialogues on the key technology paths and application scenarios of artificial intelligence. At the "Smart Healthcare and Biological Systems: Imaging, Function and Simulation" forum,Professor Li Jianping, Vice President of Peking University First Hospital, Director of the Institute of Cardiovascular Medicine, and leader of the Peking University First Hospital-Zhiyuan Joint Laboratory, spoke on the topic of "Methods and Difficulties of Clinical Myocardial Ischemia Prediction".Shared new explorations and practices of AI in the diagnosis of coronary heart disease and prediction of clinical myocardial ischemia.
As Professor Li Jianping said, "It is precisely because of the clinical demand that we use new technologies to solve difficulties, bottlenecks and pain points." At present, Professor Li's team has used AI technology to produce many important papers on myocardial ischemia, providing new ideas for the diagnosis and treatment of patients with coronary heart disease, and broadening the focus from the heart to the kidneys, hoping to make AI play a greater value in clinical medicine.
HyperAI has compiled and summarized Professor Li Jianping’s in-depth sharing without violating the original intention. The following is the transcript of the speech.
This year is the sixth Beijing Zhiyuan Conference, but it is my first time to attend. As a cardiologist, I was particularly shocked when I entered the venue. Today, I saw that all the venues were full, and some guests even stood to attend the conference. I can feel the enthusiasm and passion of everyone to welcome and embrace new technologies. In fact, both Peking University Hospital and our department have paid attention to the application of new technologies very early. I am also fortunate to take this opportunity to report my work to you.
The topic of my speech is "Methods and difficulties in clinical prediction of myocardial ischemia."It can be seen that it is precisely because of clinical needs that we use new technologies to solve difficulties, bottlenecks and pain points.
The clinical diagnosis of stable coronary heart disease is of great significance but difficult
There are two major types of coronary heart disease. One is stable coronary heart disease, also called chronic coronary syndrome; the other is unstable, also called acute coronary syndrome. The most typical example is acute myocardial infarction. For acute coronary syndrome, even after rescue, the prognosis may not be good, but the clinical prognosis of patients with stable coronary heart disease is relatively good.
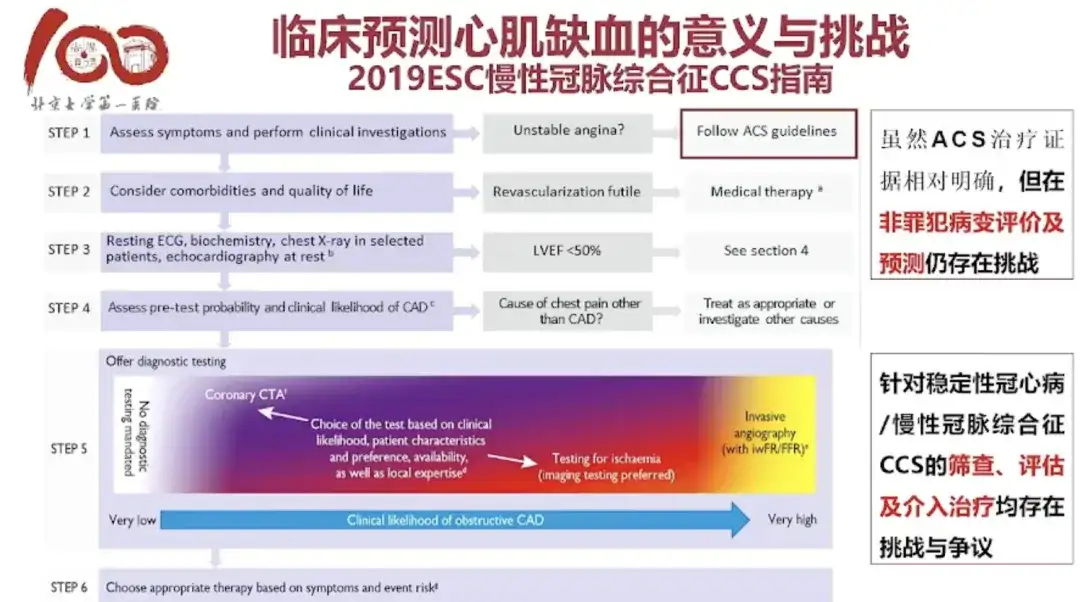
From a diagnostic point of view, even the most severe acute coronary syndrome, including acute myocardial infarction and unstable angina, is relatively easy to diagnose clinically, and the treatment indications and prognosis are relatively clear. However, there are still controversies in the diagnosis and treatment of patients with chronic coronary syndrome.The diagnostic methods for this group of people are mainly divided into two categories: non-invasive and invasive. How to choose better diagnostic and examination methods involves many issues.We pay special attention to patients with stable angina, hoping to improve the accuracy of diagnosis, intervention and prognosis of these patients.
Mainstream non-invasive diagnostic methods for stable coronary artery disease
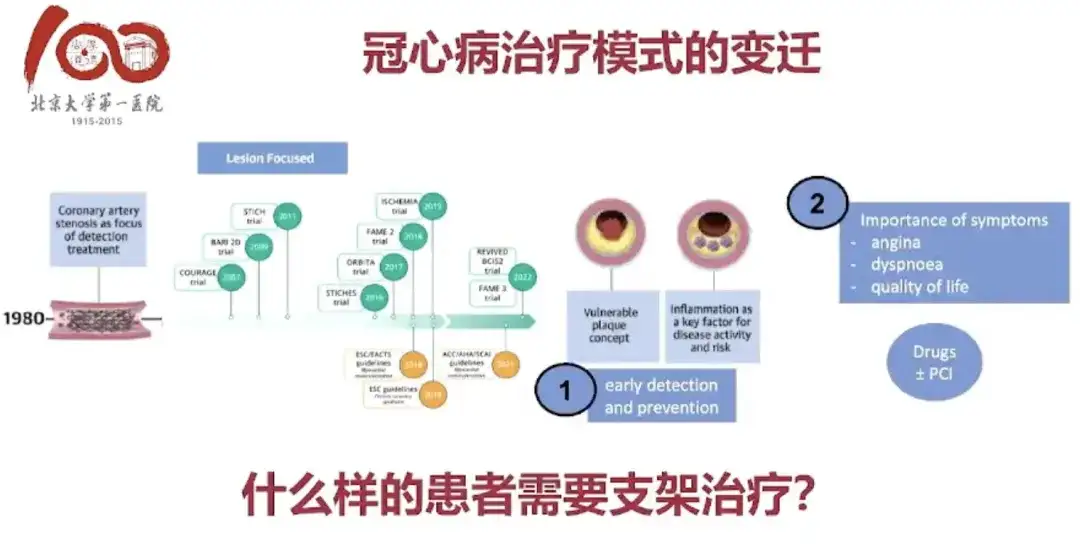
Among the treatments for coronary heart disease, drug therapy is the basis, and subsequent interventional therapy is a minimally invasive surgery. Many patients with coronary heart disease can avoid thoracotomy and bypass surgery because of minimally invasive surgery, which is a revolutionary change in treatment technology.
Although the diagnosis and treatment pathway for coronary heart disease is clear, it is also difficult to implement.At present, a large number of clinically diagnosed "coronary heart disease" actually undergo a lot of unnecessary invasive examinations. Although there are many relevant guidelines and suggestions at home and abroad, there are great differences in strategies among doctors and many difficulties are faced in the actual operation process. This urgently requires the development and promotion of non-invasive diagnostic methods for stable coronary heart disease.
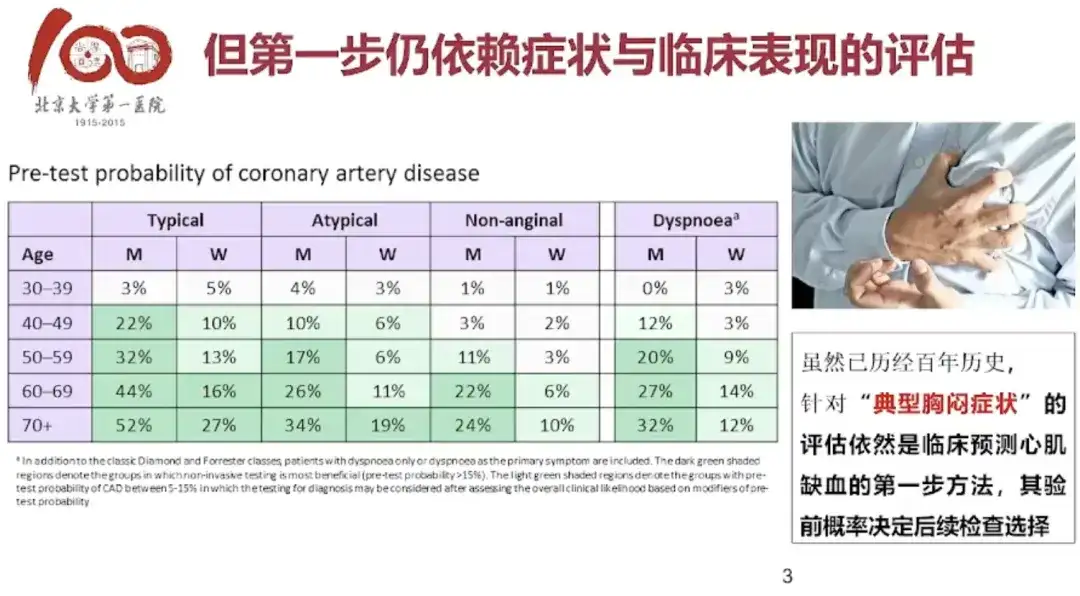
In the diagnostic process for clinically stable coronary heart disease patients in Europe, the first step is to determine whether the symptoms are typical. If it is a typical angina symptom, generally speaking, the doctor has a high degree of confidence in judging whether the patient is ill even without any examination. This is somewhat similar to the basic skills of "observation, listening, questioning and palpation" of Chinese medicine doctors. This case is actually a possibility before diagnosis, that is, judging the patient's subsequent possibility of illness and what examinations should be done next based on the patient's symptoms.
There is usually an electrocardiogram in routine physical examinations. Some doctors will diagnose patients with myocardial ischemia based on the electrocardiogram, which is actually very unscientific. Generally speaking, the electrocardiogram can only detect problems when the patient is induced to have an attack.This type of test is called an "exercise test," which involves doing an electrocardiogram while you exercise.If the ECG shows obvious ischemic changes when the patient's myocardial oxygen consumption increases, and the ECG recovers once the exercise stops, this diagnosis can determine with more than 80% whether the patient has a problem.
CTA using CT angiography is also a non-invasive technology, which is equivalent to performing coronary angiography after puncturing the patient's artery, and then using CTA to check whether the blood vessels have plaques, stenosis, and ischemia symptoms.
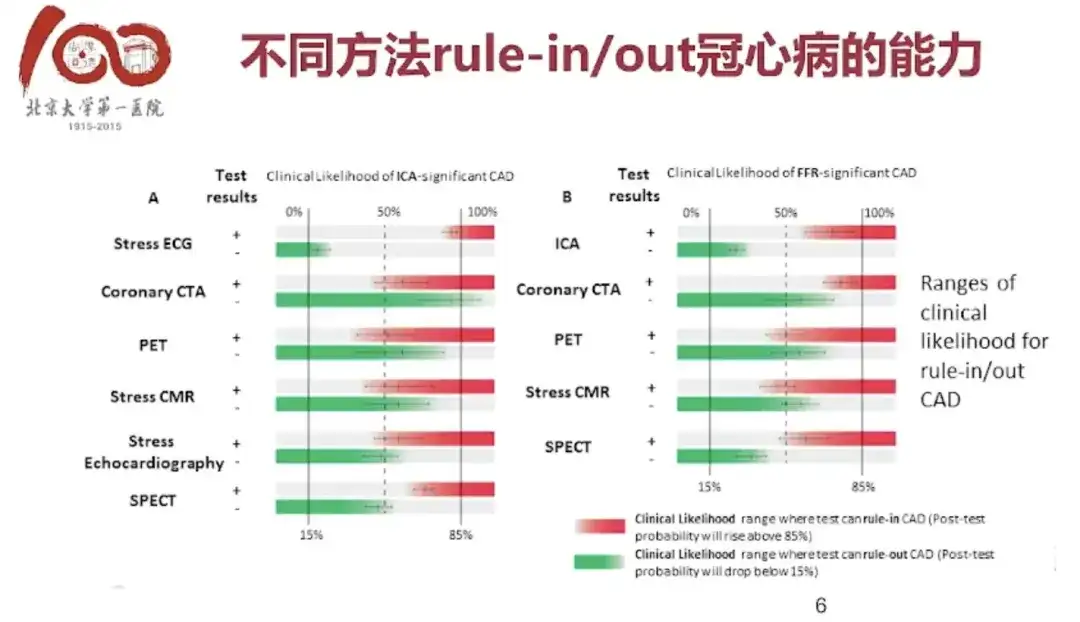
In addition, non-invasive examination methods also include stress electrocardiogram of exercise test, coronary artery CTA, stress echocardiography, stress radionuclide myocardial perfusion imaging, etc., each of which has its own accuracy in diagnosing or excluding the possibility of disease.
New technology for predicting myocardial ischemia: functional assessment
The microvessels that are connected to the distal end of the coronary artery and in contact with myocardial cells account for more than 90%, while the blood vessels seen by CTA or coronary angiography account for less than 10%. Such a large vascular bed has very good regulatory capabilities. If one side is narrow, the distal end may expand again, resulting in no ischemia of myocardial cells, which can easily lead to inaccurate assessments, and inaccurate treatments may lead to over-treatment or under-treatment.
therefore,Clinically, it is often difficult to obtain the best result when evaluating whether interventional treatment or drug treatment is better for patients with stable coronary heart disease.This is completely different from the clinical personal experience mentioned earlier.
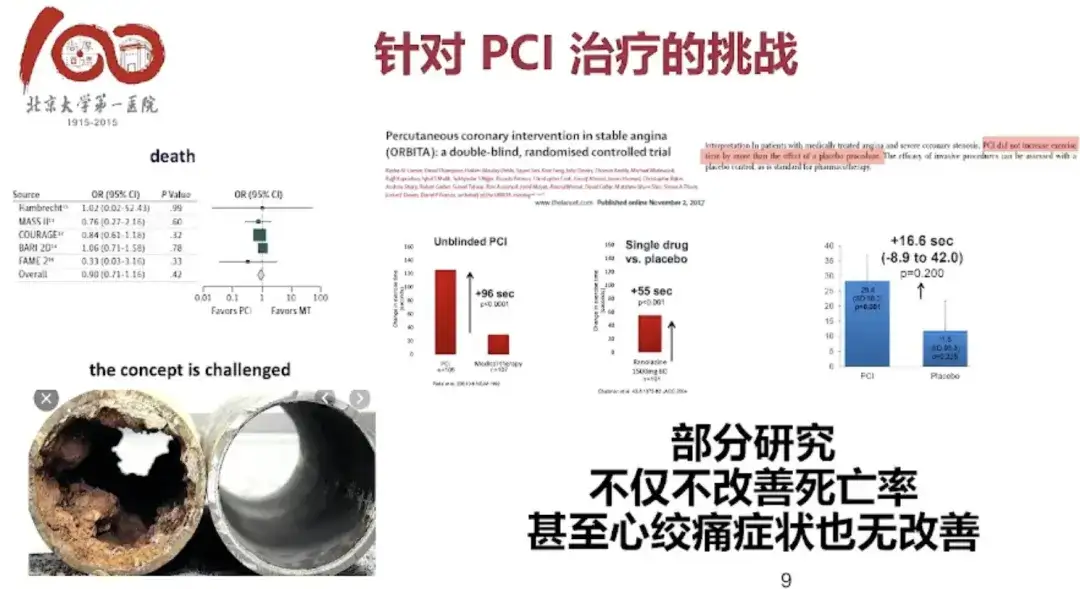
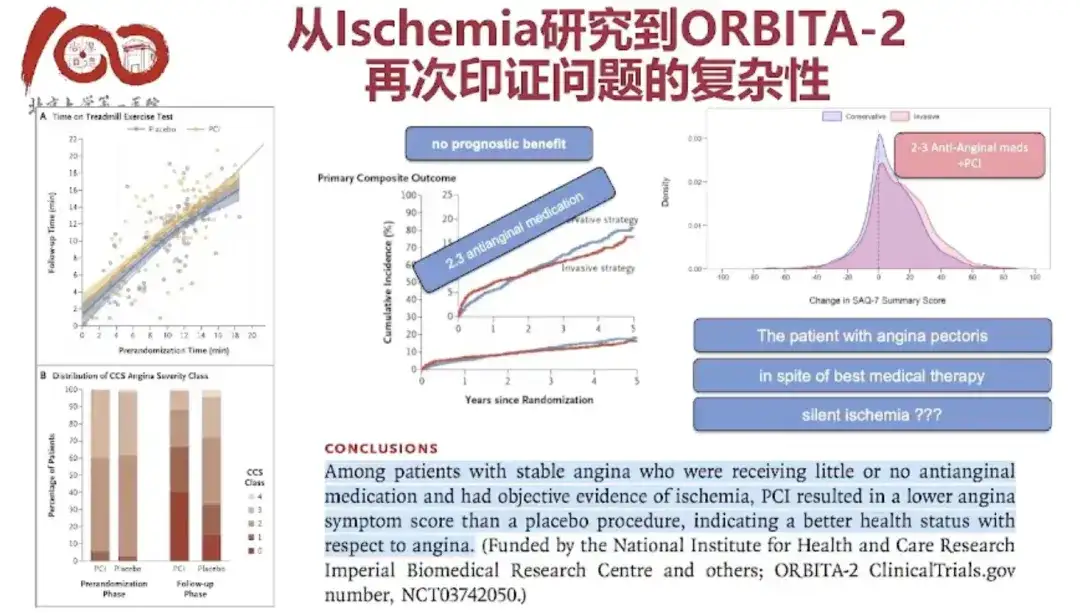
For patients admitted to the clinic, if we judge that they should undergo coronary angiography and stent treatment, many patients will benefit significantly from the treatment and their symptoms will be significantly improved. However, in clinical research, if a large-sample randomized controlled study is conducted, it will be found that interventional treatment does not show much advantage over optimized drug treatment. Even if we put one or two stents in the patient, it can further improve the patient's condition and improve the patient's quality of life, but there is no obvious benefit in improving hard indicators such as recurrent myocardial infarction and death.
The most fundamental reason is that we did not make a good functional assessment of the patient's coronary ischemia.
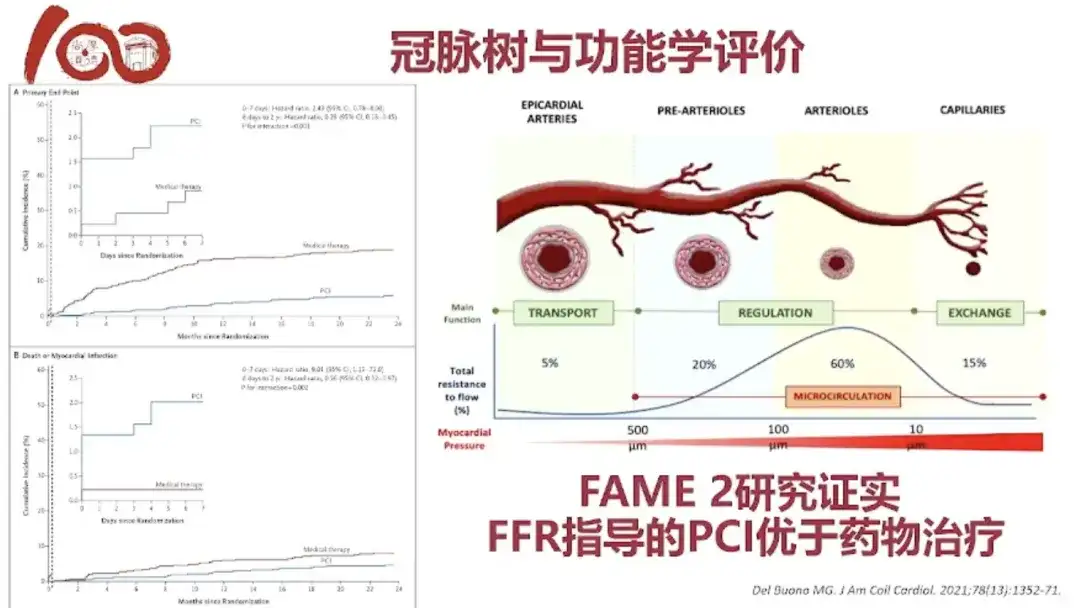
Coronary arteries range from thick to thin. Small coronary arteries are only less than 100 microns and cannot be seen during coronary angiography, but these small coronary arteries account for the vast majority of the total.
therefore,We have functionally guided treatment for coronary arteries, the FAME series of studies,The pressure receptor is placed at the stenosis of the coronary artery through a pressure guide wire. For example, if there is a 70% stenosis on the blood vessel, when we place the pressure receptor at the distal end of the lesion, the microcirculation can have a regulatory function. By expanding the microcirculation to the maximum extent, the pressure gradient of the blood before and after the lesion caused by the lesion is exposed. If the pressure gradient is large, it indicates that there is ischemia.
Myocardial ischemia functional assessment combines production and research, and has achieved fruitful results

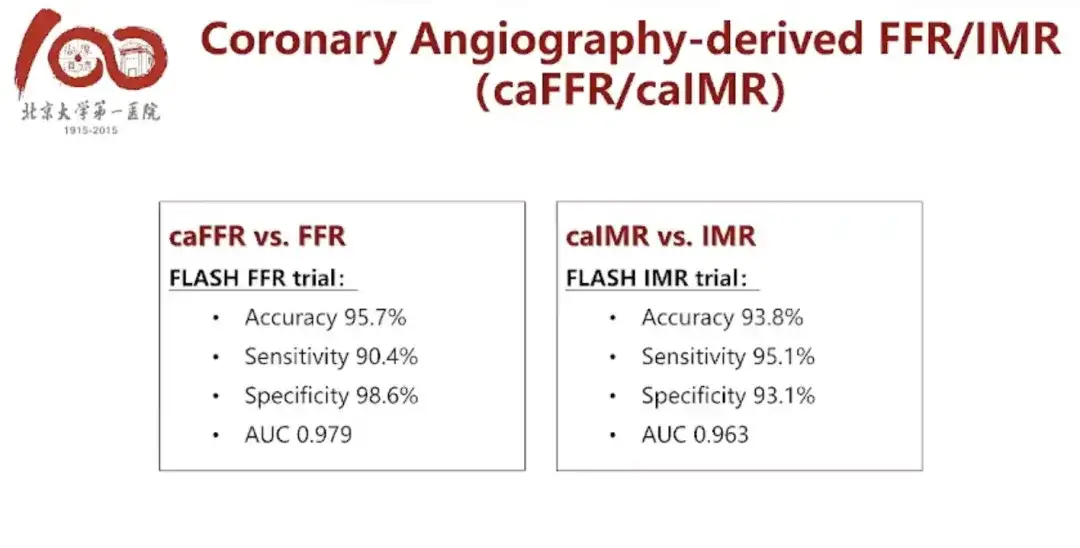
In the past, we did caFFR based on coronary angiography. The advantage of caFFR is that it does not require a pressure guidewire and the function can be calculated through an algorithm.Of course, CTFFR can go a step further and calculate FFR before angiography is performed.
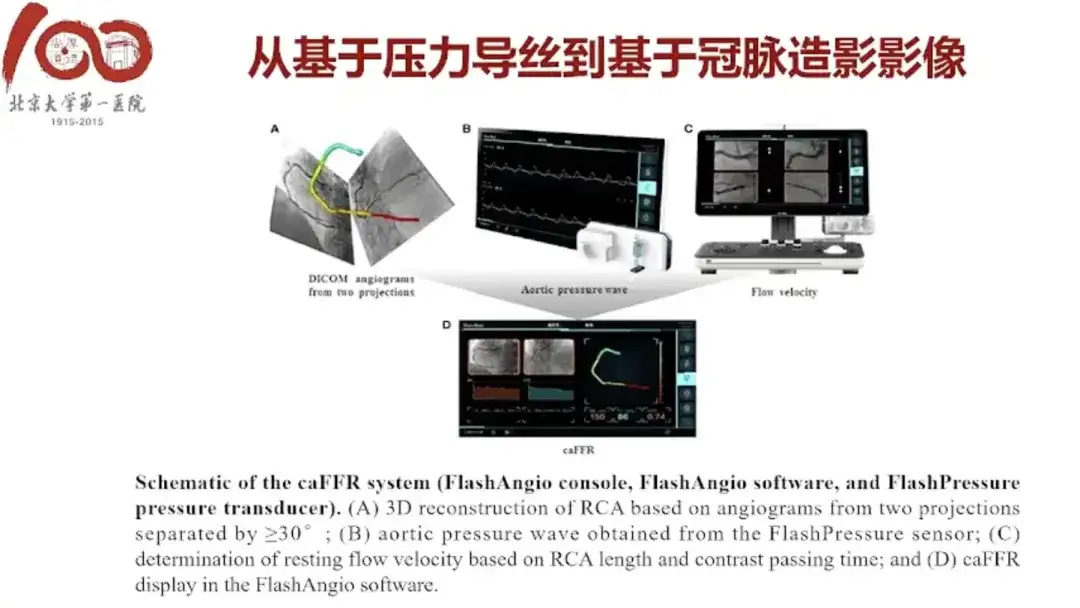
* Paper title: Accuracy of computational pressure-fluid dynamics applied to coronary angiography to derive fractional flow reserve: FLASH FFR
* Paper link:10.1093/cvr/cvz289
caFFR is a product that we developed through collaboration with companies and that has already been launched on the market, and we have published some excellent articles on it.
* Report:https://www.leaderobot.com/news/2059
* Paper Title: Coronary Angiography-Derived Index of Microvascular Resistance
* Paper link:10.3389/fphys.2020.605356
We have also obtained a key project of Beijing's first launch fund, which mainly evaluates IMR based on myocardial strain. IMR is the microcirculation resistance index.
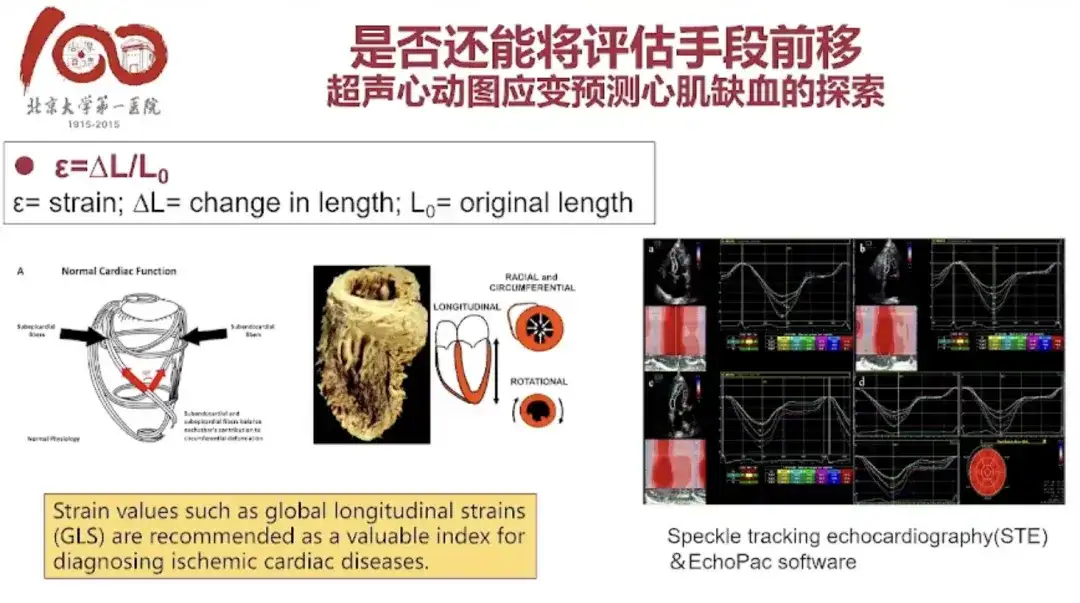
Professor Zhu Tiangang is a domestic ultrasound expert. Echocardiogram is a very simple value on ultrasound, called "myocardial strain". The beating of the heart is not like a balloon blowing up and shrinking, but during the contraction process, countless myocardial cells are doing very complex mechanical coordinated movements, which will lead to the most effective blood pumping movement like twisting a towel. We can also reflect the presence of myocardial ischemia by measuring such myocardial strain.
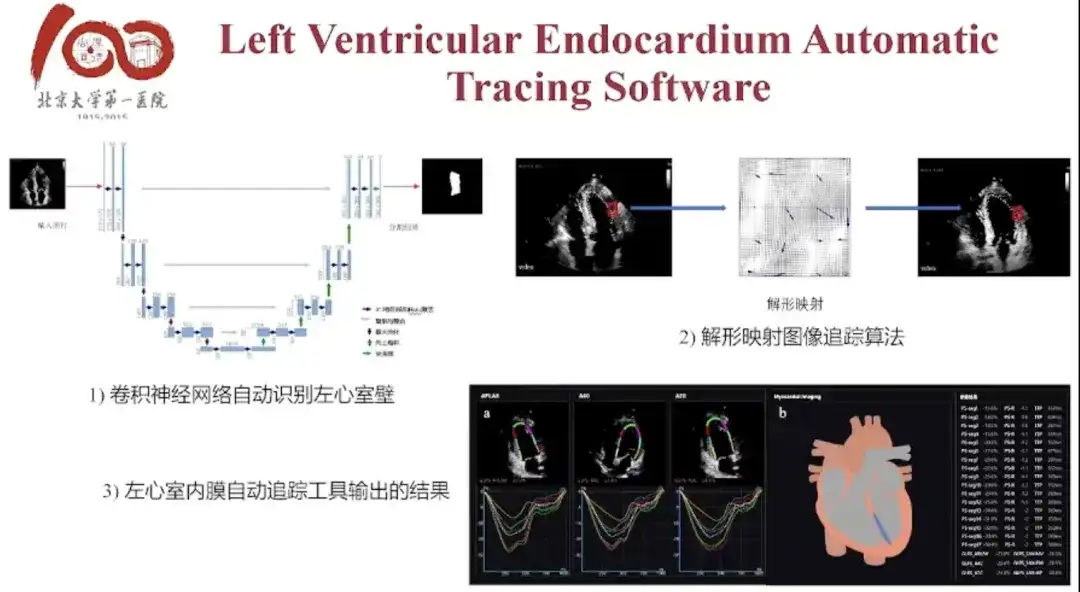
Left Ventricular Endocardium Automatic Tracing Software is a preliminary result of our collaboration with the artificial intelligence teams of the University of Georgia and Tsinghua University based on our own data. The results of the research design were quite good at the time.Myocardial strain has achieved relatively ideal results in predicting myocardial ischemia.
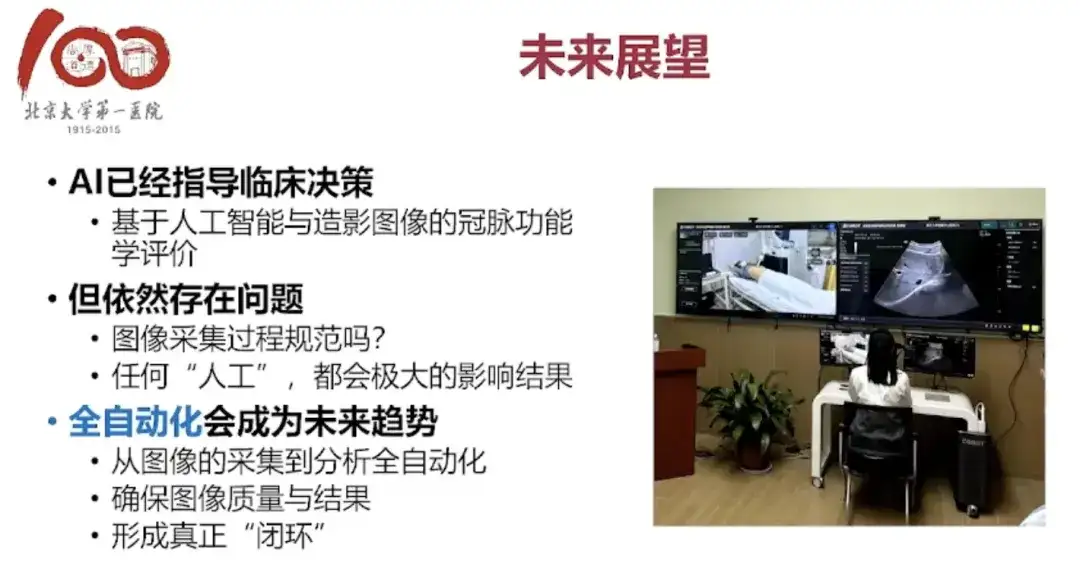
Regarding ischemia, we have focused on the kidneys from the heart. The renal artery also has stenosis problems, and the kidneys also have ischemia problems. We found that there are indeed many opportunities, but also many challenges.My personal feeling is that this field requires interdisciplinary talents.Although there is now cross-integration between medicine and engineering, and we have established a joint laboratory for artificial hearts with Zhiyuan, we still feel that clinical doctors are not sufficiently involved in this regard. We hope to have more in-depth cooperation with professionals, and we also hope that talented people in this area can join our hospital.
About Professor Li Jianping

Professor Li Jianping graduated from Peking University Medical College with a degree in clinical medicine in 1992, and received a doctorate in cardiovascular medicine from Peking University First Hospital in 1998. He worked as a postdoctoral fellow at Harvard University from 1999 to 2003. Since returning to China in 2003, Professor Li Jianping has been mainly engaged in the interventional diagnosis and treatment of coronary heart disease. He is a coronary heart disease intervention instructor of the Chinese Cardiovascular Disease Interventional Diagnosis and Treatment Training Program and a member of the Expert Committee of the Beijing Cardiovascular Intervention Quality Control and Improvement Center.
Professor Li Jianping is mainly engaged in interventional treatment of coronary heart disease, and conducts clinical and basic research on hypertension, coronary heart disease and other atherosclerotic diseases. In the areas of H-type hypertension and primary prevention of stroke, non-invasive coronary artery functional assessment, and the study of fine particulate matter in air pollution and the mechanism of early atherosclerosis, he conducts research based on the characteristics of the Chinese population, innovates theory and practice, realizes industrial transformation, and makes outstanding contributions.
In the field of scientific research, Professor Li Jianping has published many academic papers in top cardiovascular journals such as JAMA, Cardiovascular Research, and ATVB. He has won four research awards in this field as the second finisher, including the second prize of the 2011 Chinese Medical Science and Technology Award for "Preventing stroke in Chinese people by lowering blood pressure and reducing plasma homocysteine levels", the first prize of the 2012 Huaxia Medical Science and Technology Award for "Translational medicine research on the prevention and treatment of stroke in H-type hypertension", the first prize of the 2016 Science and Technology Progress Award for Outstanding Scientific Research Results in Higher Education Institutions for "Research and transformation of the causes of high incidence and precise prevention of stroke in China", and the second prize of the 2016 National Science and Technology Progress Award for "Translational application of precise prevention strategies for stroke in China". He presided over many research projects such as the major projects of the Ministry of Science and Technology, the National Natural Science Foundation, and the First Fund.