Command Palette
Search for a command to run...
Led by Peking Union Medical College Eye Hospital, Five Ophthalmology Centers Work Together to Use AI to Assist in the Detection of 13 Types of Fundus Diseases

Eyes can cause a variety of diseases. Airdoc The jointly released "Blue Book of Health of Four Million People Undergoing Physical Examination" shows that the total detection rate of fundus abnormalities has increased year by year in recent years, from 76.1% in 2019-2020 to 78.7% in 2022-2023. The incidence of fundus diseases continues to rise and has become the most common irreversible cause of blindness worldwide.
Since the diagnosis of ophthalmic diseases is highly dependent on image recognition, ophthalmology is very suitable for the application of technologies such as deep learning. In order to further explore the potential value of deep learning in the diagnosis of fundus diseases,Led by Chen Youxin, director of the Department of Ophthalmology at Peking Union Medical College Hospital, five ophthalmology centers across the country (Department of Ophthalmology at Peking Union Medical College Hospital, West China Hospital of Sichuan University, The Second Hospital of Hebei Medical University, Tianjin Medical University Eye Hospital, and Wenzhou Medical University Eye and Optometry Hospital) in collaboration with Beijing Zhiyuan Huitu Technology Co., Ltd. and Professor Li Xirong of the School of Information at Renmin University of China, developed a deep learning system (DLS) to help junior ophthalmologists improve their diagnostic consistency by approximately 12%, providing a new method for the automatic detection of 13 major fundus diseases.
Research highlights:
* This study was conducted as a prospective clinical trial to evaluate the diagnostic performance of DLS in assisting primary ophthalmologists in detecting 13 major fundus diseases.
* After using DLS, the diagnostic consistency of primary ophthalmologists improved by approximately 12%
* DLS should be able to detect at least one existing disease, which is consistent with the original intention of defining a new indicator

Paper address:
https://doi.org/10.1038/s41746-023-00991-9
Follow the official account and reply "DLS" to get the complete PDF
DLS: Opening up new ideas for diagnosing fundus diseases
Dataset: Collect fundus images to ensure accurate results
Compared with previous studies, this study collected more color fundus photography data, expanding the total amount of data to 81,395 images (77,181 images in the training set, 1,087 images in the validation set, and 3,127 images in the test set).
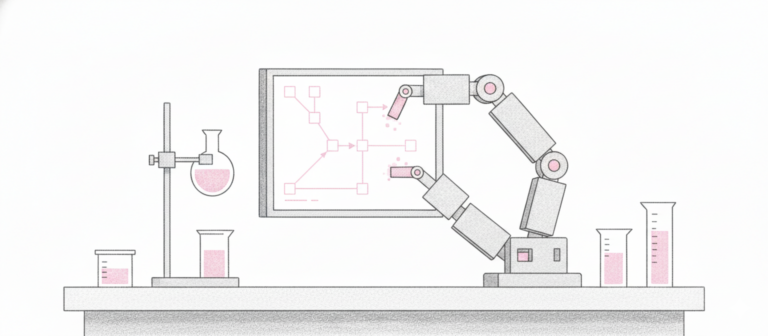
Model composition: Two major research models, collaborative construction process
DLS consists of two parts: the image quality assessment model and the diagnostic model. The workflow is shown in the figure below:

The image quality assessment model is a regression model based on ResNet-34 CNN.By inputting a single fundus image, the image quality assessment model is used to determine whether the image quality is suitable for diagnosis. If it is suitable, the diagnostic model will generate diagnostic suggestions; otherwise, the system will issue an alarm, indicating that the image quality is not suitable for diagnosis, but the system cannot provide diagnostic suggestions.
The fundus disease diagnosis model is an extension of previous work, with the CNN model seResNext50 as the main structure.The fully connected layer is designed with two branches to determine whether a disease is present and which specific disease is present. To better stabilize the prediction results, the study trained 3 parallel seResNext50 models with late fusion.
Research design: Five major hospitals work together to ensure reliable results with multiple factors
This study was conducted in five tertiary hospitals, including Peking Union Medical College Hospital, West China Hospital of Sichuan University, The Second Hospital of Hebei Medical University, Tianjin Medical University Eye Hospital, and Wenzhou Medical University Eye Hospital.From August 2020 to January 2021, a total of 750 participants were prospectively screened, of whom 748 completed all surgeries. The participants were all outpatients aged between 18 and 75 years, with an average age of 51.7 years. There were 152 cases of diabetes (20.3%), 216 cases of hypertension (28.9%), and 104 cases of hyperlipidemia (13.9%). Among them, there were 324 male patients (43.3%). They all went to any of the five hospitals for fundus imaging examinations, had complete medical records, and underwent comprehensive ophthalmological examinations.
The study invited six ophthalmologists (associate professors with at least five years of experience) to annotate the images, and the final diagnosis was determined by their discussion. In addition, nine junior ophthalmologists (residents or attending physicians with less than three years of experience) received training and read the images for evaluation in the study.
After a one-week washout period, they annotated the same set of images again, which were randomly reordered and labeled with the labels previously annotated by DLS to form the experimental group. At the same time, each junior ophthalmologist was assigned to independently annotate part of the dataset as a control group. In addition, all fundus images in the group were labeled as DLS group by DLS.
The subset of images that can be fully analyzed in this study is 1,493 images, of which 477 (32.0%) were marked as normal fundus according to the annotations and discussions of 6 senior ophthalmologists. Another 1,016 (68.1%) images were marked with diseases, of which 1,386 (92.8%) were marked with only one disease, 78 (5.2%) were marked with two diseases, 29 (1.9%) were marked with three diseases, and a total of 251 (16.8%) images were marked as "other abnormalities".

Fundus images were obtained by skilled technicians using both (non) dilated pupilsFundus CameraSampling was performed using standard operating procedures to ensure image quality for subsequent annotation and reading.

The selection of diseases for this study was based on their prevalence and threat to visual function, while also considering the clinical potential for screening using fundus images. Ultimately, the study selected 13 major fundus diseases with standard diagnostic criteria, including referable diabetic retinopathy (DR),Retinal vein occlusion (RVO), retinal artery occlusion (RAO), pathological myopia, retinal detachment (RD),Primary retinitis pigmentosa (RP), atrophic and neovascular age-related macular degeneration (AMD), epiretinal membrane (ERM), macular hole (MH),Central serous chorioretinopathy If the image contained signs of other diseases that were not included in the selected 13 diseases, it was classified into the category of “other fundus abnormalities”.

Experimental results: DLS can effectively detect specific fundus diseases, but it can also affect the accuracy of diagnosis
Compared with the control group, the annotations of 888 (59.4%) images were changed by junior ophthalmologists. Among them, 801 (53.5%) images were modified according to the suggestions of AI. Although in some cases, junior ophthalmologists mistakenly changed the correct diagnosis decision to an incorrect label based on the suggestions of DLS, they did get a lot of help from it.

Blue means the label is changed to an incorrect diagnosis label, and red means the label is changed to a correct label
The study stated that this is the first clinical trial to prove that DLS can help junior ophthalmologists significantly improve diagnostic consistency in the detection of a variety of major fundus diseases. It also proves that the DLS-assisted multiple fundus disease screening image reading model for junior ophthalmologists is an effective clinical method.
In this study,The overall disease diagnostic sensitivity and specificity of DLS were 96.6% and 81.8%, respectively.It can effectively detect specific fundus diseases, detect fundus abnormalities, and assist in referring patients for specialized investigations and evaluations. In addition, high specificity helps reduce unnecessary referrals and medical costs.
This study set up three control groups, namely the AI-assisted doctor reading group (experimental group), the doctor independent reading group (control group) and the AI reading group (AI group).
The results showed that the diagnostic consistency rates of the experimental group, control group and AI group were 84.9%, 72.9% and 85.5% respectively, that is, with the assistance of AI,The image reading and diagnostic ability of junior physicians can be improved by approximately 12%.In this study, the diagnostic consistency between the experimental group and the DLS group was similar, which suggests that DLS alone can be fully effective. However, it is still crucial to involve human doctors. Although AI-based disease screening and identification has been widely used in actual clinical practice, it also introduces risks such as misdiagnosis.
In addition, in this study, the sensitivity of the experimental group and the control group to fundus diseases was comparable, and the experimental group was significantly better than the control group, especially for diseases including suspected GON, optic atrophy, atrophic AMD, and CSC. These results show thatJunior ophthalmologists are able to distinguish between abnormal and normal fundus, but they still lack the ability to diagnose specific diseases. This shortcoming can be addressed with the assistance of DLS, thereby greatly reducing the missed diagnosis rate and also reducing the limitations on the degree of specialization of junior ophthalmologists in diagnosing fundus diseases.
However, the diagnostic accuracy of the control group (60.5%) was higher than that of the experimental group (44.2%). By reviewing the annotations, the study found that DLS tends to annotate more labels for an image, which will help reduce the missed diagnosis of junior ophthalmologists, but will also affect the accuracy of the diagnosis.
In addition, this study still has certain limitations. First, although the dataset selected real images of fundus diseases, some categories only contained a small number of images, which may lead to biased results, and all participants were Chinese Han patients. In future work, it is necessary to further expand the prospective dataset and enrich the types of patients.
Secondly, some of the diseases selected in this study require collection from the peripheral area of the retina, which is beyond the range of fundus images. Therefore, DLS cannot detect them in the initial stage. The study used wide-field color fundus photography, which can solve this problem to a certain extent.
Third, since the diagnostic ability of junior ophthalmologists has been greatly improved with the help of DLS, this technology can also be used as an application scenario for educational purposes, which is also a meaningful topic that needs to be more comprehensively investigated and evaluated in future work.
Professor Chen Youxin is deeply engaged in ophthalmology and promotes the application of AI
"How great is Peking Union Medical College Hospital?" - This is an active post on a Chinese social media, with countless replies using rare cases to prove the superb medical skills of Peking Union Medical College Hospital. As the "Vienna Eye Center of the East", the Ophthalmology Department of Peking Union Medical College Hospital has long been active in the first echelon of the industry. Its current director, Chen Youxin, can be said to be a witness and creator of the development history of ophthalmology in China.
In 1993, Dr. Chen Youxin, who had just entered the field of ophthalmology, came to Union Hospital as a doctor of ophthalmology under Professor Zhang Chengfen. In 2001, Professor Chen Youxin, who was studying in the United States, received an email from Professor Zhao Jialiang, the then chairman of the Ophthalmology Branch of the Chinese Medical Association, who hoped that he could return to China as soon as possible to help prepare for the 8th National Ophthalmology Academic Conference the following year. After careful consideration,Chen Youxin eventually terminated his studies early and chose to return to China to build the National Ophthalmology Annual Conference, a platform that later helped countless Chinese ophthalmologists broaden their horizons.
Professor Chen Youxin has been working on fundus medicine for a long time. In 1982, Professor Yannuzzi of the United States first reported and named a fundus disease at a meeting of the Macula Society: idiopathic polypoidal choroidal vasculopathy (PCV). As the research deepened, scholars found that the disease had the highest incidence in the Asian population, and the large population base also led to a large number of patients with this disease in my country. In 2017, the first "PCV Research Alliance" in the Chinese ophthalmology community, initiated by Professor Chen Youxin, was established.
Subsequently, Professor Chen Youxin led a number of domestic institutions to carry out the START study, a real-world study of Conbercept ophthalmic injection in the treatment of PCV.The "Establishment and Theoretical Innovation of the Diagnosis and Treatment System for Polypoidal Choroidal Vasculopathy" led by Professor Chen Youxin's team won the second prize of the 2022 China Medical Science and Technology Award.
also,Li Bing, the first author of this paper, studied under Professor Chen Youxin and Professor Ye Junjie, an ophthalmologist at Peking Union Medical College Hospital.He is currently a resident physician in the Department of Ophthalmology at Peking Union Medical College Hospital. He has published more than 10 papers in SCI and Chinese core journals as the first author, and has given reports at academic conferences such as the National Ophthalmology Annual Meeting and the National Fundus Disease Meeting.
In terms of AI-assisted identification of fundus diseases, Peking Union Medical College Ophthalmology is at the forefront of the times. As early as 2021, Professor Chen Youxin had successfully identified multiple diseases such as venous occlusion, diabetic lesions, and macular degeneration through artificial intelligence, which also received a grant of 5 million yuan from the Beijing Municipal Key Project.
At present, the Ophthalmology Department of Union Hospital has carried out research on the application of artificial intelligence in ophthalmic disease screening, treatment prediction, correlation between eye and systemic diseases, multimodal and wide-angle fundus lesions and multi-disease lesion identification, and has been applied and promoted in many grassroots scenarios, providing ideas and solutions to solve the problem of difficulty and high cost of medical treatment caused by the uneven development of medical resources.
In Professor Chen Youxin's view, all efforts are aimed at sinking medical resources to the grassroots and providing better diagnosis and treatment for patients far away from big cities. With the development of technologies such as artificial intelligence, Professor Chen Youxin's efforts have begun to bear fruit, and in the future, he will continue to overcome difficulties and continue to exert the power of artificial intelligence in the pathogenesis, pathogenesis, diagnosis and treatment of related diseases.
References:
1.https://mp.weixin.qq.com/s/zctJN7Q7PYjsPypkStWcoA
2.https://mp.weixin.qq.com/s/LoXWmWVpYnrr1-vKBrpL6A
3.https://mp.weixin.qq.com/s/IFS5JWIyb_5mqfJccAQO2g
4.https://mp.weixin.qq.com/s/zxP9n_vGWNcH2rPW-dq37g
5.https://www.pumch.cn/detail/34540.html